How common are suicide and self-harm?
The incidence of suicide in Ireland is about 11 per 100,000 (CSO, 2015). While this is not an exceptionally high rate in the international context, the suicide rate among young people in Ireland is among the highest in Europe (Eurostat, 2015) The rates of suicide in men are about four times higher than the rates in women. Conversely, rates of non-fatal self-harm are consistently higher in women. The most common means of suicide is hanging (approximately 80%), while the most common methods of non-fatal self-harm are intentional overdose, self-cutting, and attempted hanging. Alcohol is involved in up to one-half of suicides and one-third of non-fatal self-harm presentations. To read more on the epidemiology of suicide and hospital-treated self-harm in Ireland, visit here.
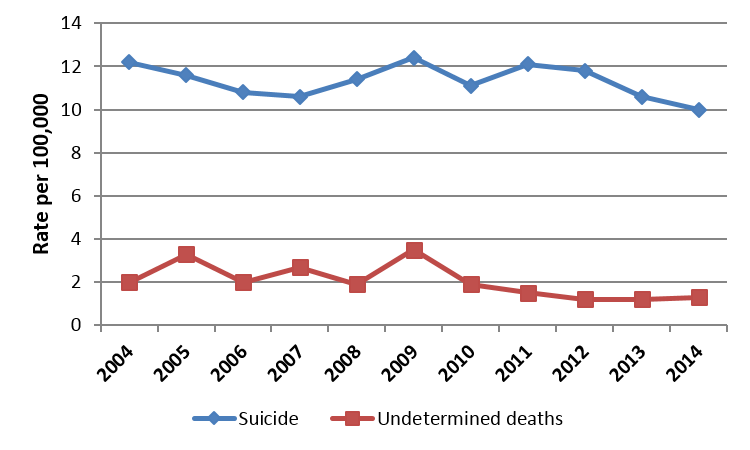
Source: CSO, 2015; NSRF, 2015
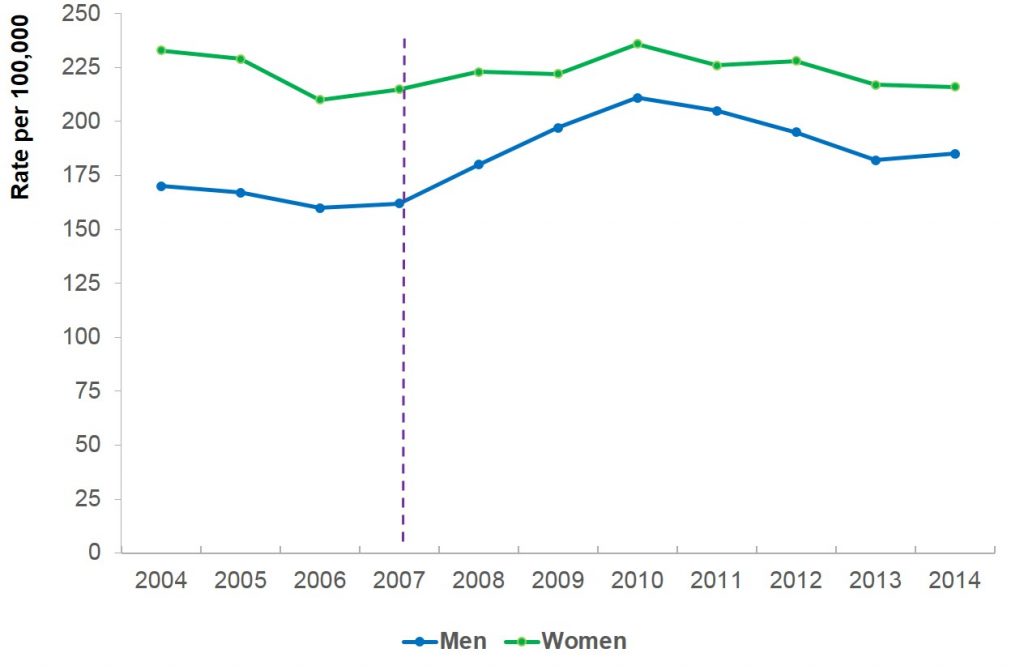
Source: NSRF, 2015
What are the risk factors for suicide?
There are certain characteristics that place a person at elevated risk of suicide:
- Young and middle aged men; people who are economically disadvantaged, and people who are homeless
- Suicidal thoughts or a history of self-harm or suicide attempts
- Substance abuse problem, such as alcohol or drug abuse
- Psychiatric disorder, most often major depression, post-traumatic stress disorder or bipolar disorder
- Family history of mental disorders, substance abuse, suicide, or violence (including physical or sexual abuse)
- Being socially isolated or a victim of bullying
- A traumatic experience during childhood, a history of sexual or physical abuse, or a history of parental neglect
- Certain medical conditions, such as chronic disease, chronic pain or terminal illness
These risk factors are less prominent factors which confer vulnerability for suicide. They should not be used to ascertain whether a person is at imminent risk of suicide.
How does a person come to take his/her own life?
The causes of suicide are complex, involving the interaction between longer standing vulnerability or diathesis and precipitant stressors, as outlined in the Integrated Motivational-Volitional Model of Suicidal Behaviour (O’Connor et al, 2011).
The ‘diathesis’ or vulnerability refers to biological, cognitive and social predispositions that place a person at higher risk of suicide. These include genetic predisposition, traits of impulsivity or poor problem-solving, and childhood adversity, such as exposure to abuse or parental mental disorder.
The ‘precipitant stressor’ occurs closer to the time of the suicide, and may involve psychosocial crisis (such as job loss, relationship breakdown, social isolation, or financial crisis) or the onset or worsening of a psychiatric disorder.
When a stressor is experienced by someone with pre-existing vulnerabilities, the psychological pain they experience may eclipse possible solutions or future hopes. In this trapped state, they may begin to think about death or suicide as a means of escape. The nature of this suicidal ideation can range from a passive death wish to intrusive visualisations or a concrete plan. Some people with suicidal ideation do not act on their thoughts. Risk factors that place a person at higher risk for translating ideation into suicidal behaviour include:
- A history of self-harm
- A suicide plan
- Trait impulsivity
- Previous exposure to suicide modelling in peers or family
- Access to a means of suicide (such as medication, a ligature or firearm)
- Being alone or unsupervised
- Consuming alcohol or other drugs that reduce behavioural inhibition
A person with an imminent intention to harm themselves should be treated as a medical emergency. There is more information on assessing and responding to suicide risk here.
Source: O`Connor et al, 2011