A death by suicide affects many people, including their GP. The majority of people who die by suicide have been in contact with primary care services in the year before death. The suicide may come as a shock to the GP, or as the inevitable ending to a long story of adversity. Whatever the link and relationship was to the patient, it is important to take the time to integrate the death, professionally and personally. Research suggests that health care practitioners need a personal or professional support system to help them cope in the aftermath of suicide. Try to link in with peers who have had similar experiences and understand how they came to terms with the death. It may be helpful to speak with a mentor or seek therapeutic support to prevent burnout or stress. Take time to grieve the patient, and be patient with yourself if you have feelings of anger, frustration or disappointment. Depending on the context of the death and the personal circumstances, some GPs may suffer post-traumatic stress disorder, distress, or burnout in the aftermath of a patient suicide. It’s important to seek professional help if you feel that the death is continuing to affect you.
Through the Health in Practice programme The Irish College of General Practitioners provides access to confidential GP support services, delivered by GPs and counsellors who have specific training in providing GP services to colleagues.
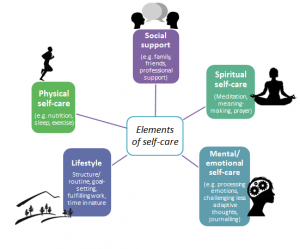
In the context of a busy general practice, GPs are encouraged to engage in broader self-care, paying attention to your physical, social, emotional and spiritual wellbeing.
Conversation with a GP: Self-care and Peer Support for GPs
In the video below Professor Colin Bradley, Head of the Department of General Practice University College Cork, outlines the importance of self-care for GPs when dealing with self-harm and suicide, how to deal with challenges and the support services available.