Effective treatments for suicidal behaviour and depression > |
Asking about suicide
Asking a person whether they have experienced suicidal ideation or behaviour can be difficult. A mental health professional may be worried that this question may prompt suicidal ideation, may affect rapport with the client, or result in a disclosure that is complicated to manage.
On the contrary, there is strong evidence from a systematic review (Dazzi et al, 2014) that asking about suicidal ideation does not render a person more likely to experience ideation, and indeed reduces feelings of distress at follow-up. This suggests that asking a client about suicidal ideation or behaviour will not prompt suicidal ideation or increase distress, but rather creates a valuable opportunity to intervene with people at risk of translating suicidal ideation into action. Of course, suicide bereaved clients may have an additional resistance to disclosing ideation, given the effect the aftermath of their family member’s death. However, the mental health professional can reassure the client that this is the very reason why these issues should be discussed.
Given the research evidence that asking about suicidal ideation is safe and necessary, the next issue is how to actually initiate this discussion. Some clients may spontaneously speak about death wishes, fleeting suicidal ideation, or a suicide plan. Others may make opaque references, such as ‘if I’m still around’ or others being ‘better off without me’. Some clients may not express ideation but rather manifest hopelessness (perceiving themselves as intractably trapped), low mood, insomnia, or a desire for medication change. A mental health professional can initiate the discussion, asking whether the client has had any thoughts of harming themselves in this difficult situation. With any allusion to death or suicide by the client, the mental health professional can probe further, asking about the frequency and intensity of these thoughts, whether the person has a certain plan of what they would do, and whether they have done anything already to enact suicidal behaviour. Previous acts of self-harm are one of the strongest predictors of future suicidal behaviour, and previously engaging in high lethality attempts (such as attempted hanging) confers high risk of death by suicide in the future. Other preparations for suicide to enquire about include preparations for the act itself (researching methods, stockpiling medications, or procuring a weapon or ligature) or preparations for death (such as writing a will or suicide note, saying farewell, or making arrangements).
If a client has a concrete plan, cannot distance themselves from their suicidal ideation, or have put preparations in place, they may be at imminent risk of suicide. This should be treated as a medical emergency, and psychiatric admission should be seriously considered for the duration of the crisis.
Sometimes, a client’s risk might be high but not imminent: where ideation is less prominent but the client has other risk factors (previous suicidal behaviour, lack of social support, worsening psychiatric illness or substances abuse, male gender, or few protective factors such as positive future plans). Arrangements should be made for psychotherapeutic or pharmacological treatment with short follow-up periods.
If a mental health professional has experienced client suicide, they might feel as if suicide is very difficult to predict and prevent. However, the majority of people who are kept safe, survive a suicidal crisis, subsequently receive the required treatment, and do not go on to die by suicide.
Effective treatments for self-harm and depression
In this video Professor Eugene Cassidy, Consultant Liaison Psychiatrist and Clinical Professor University College Cork/Cork University Hospital, outlines evidence based interventions for people with depression and for people who have engaged in self-harm.
Treatments to prevent self-harm repetition
For clients with Borderline Personality Disorder, Dialectical Behaviour Therapy is effective in reducing suicidal ideation, self-harm and suicide. DBT reduces the frequency of self-harming behaviour in Emotionally Unstable Personality Disorder but not the likelihood of suicidal behaviour occurring compared to standard care. It is an intensive intervention delivered by clinical psychologists and is now widely available through mental health services in Ireland.
There is also good evidence for the effectiveness of cognitive-behavioural therapy in preventing future self-harm. A CBT intervention designed to address self-harm (Slee et al, 2008) was effective, particularly so in the group of participants with a history of sexual abuse. Mindfulness-based cognitive therapy appears to be particularly useful in preventing relapse in depressed clients with a history of suicidality. However, it must noted that not all people are suitable for CBT.
A recent Cochrane review found no clear evidence for the effectiveness of antidepressants, antipsychotics, mood stabilisers, or natural products in preventing repetition of self-harm among those who have already presented with self-harm (Hawton et al, 2015). For children and adolescents, a Cochrane review found no clear evidence of effectiveness for compliance enhancement, individual cognitive behavioural therapy (CBT)-based psychotherapy, home-based family intervention, provision of an emergency card, or group therapy. Mentalisation therapy had a modest effect on repetition of self-harm in a small trial of adolescents (Hawton et al, 2015). A systematic review on psychosocial treatments for self-harm among adults, reported good effect sizes for cognitive behaviour therapy (CBT) (Hawton et al, 2016). This review also revealed that Dialectical Behaviour Therapy may reduce the frequency of self-harm, however, this involved only a small number of trials.
Treatments for depression
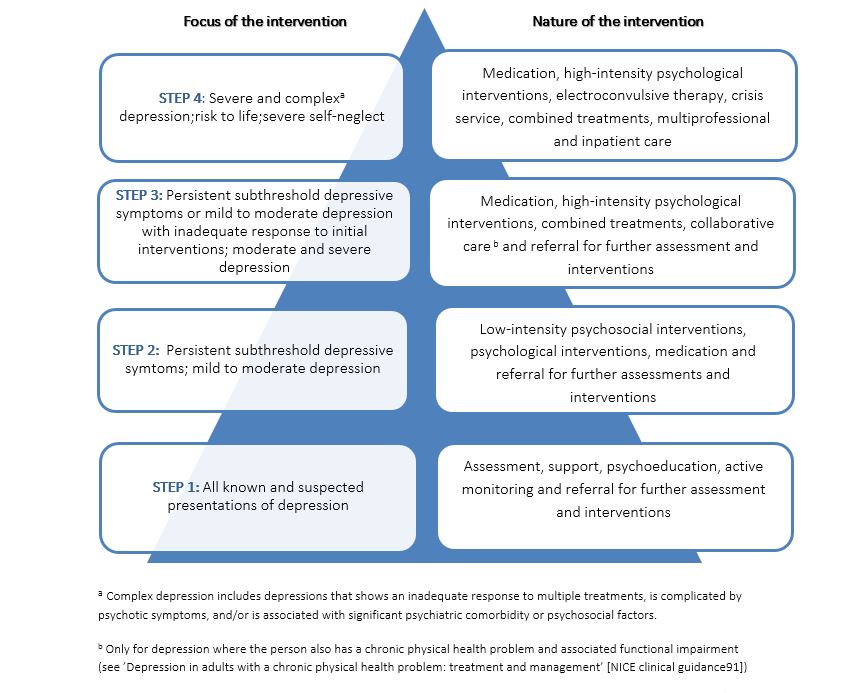
In line with the UK NICE guidelines for the treatment of depression in primary care, it is recommended that depression is treated according to a stepped approach, depending on the severity of the disorder.
When managing a client with depression, a mental health professional should educate the client about the disorder, namely that it is a disorder that is treatable (though it may take a few weeks to see an improvement), that adherence to treatment is important, and that healthy daily habits combined with treatment will lead to improvement in most cases.
Clients with depression benefit from psychotherapy. Evidence for efficacy is most consistent for cognitive-behavioural therapy (CBT). CBT usually takes place over six weeks to six months. Clients are helped to identify and challenge cognition’s that maintain depressed mood and to improve the daily balance between stress and duties versus relaxation and enjoyable activities. Other approaches with some evidence for efficacy are interpersonal therapy (IPT) and mindfulness- or acceptance-based therapies. The latter seek to teach clients to avoid self-evaluation and self-judgement based on the content of their thoughts. Person-centred counselling is non-directive and is characterised by an empathetic and supportive approach.
In Ireland 1 in 25 adults use antidepressants. (National Advisory Committee on Drugs, 2012) There are many different types of antidepressant medications, which differ more in terms of side effects than in efficacy. Two important groups of antidepressants are tricyclic antidepressants (TCAs) and Selective Serotonin Reuptake Inhibitors (SSRIs). TCAs include amitriptyline, clomipramine, dibenzepin, and doxepin, and side effects include delirium, dry mouth, and tremors. SSRIs include citalopram, escitalopram, fluoxetine, fluvoxamine, paroxetine, and sertraline (College of Psychiatry of Ireland, 2011) When introducing antidepressants to the client, it is important to inform them about possible side effects and that it may take a few weeks of taking the medication to feel relief. It is also important to make clear that antidepressants do not change one’s personality and are not addictive.
Most people will benefit from learning more about depression through psychoeducation sessions or resources, such as iFightDepression.com, or through a self-guided online CBT such as iFightDepression or Moodgym.
A client should be referred specialised psychiatric care if they are experiencing delusional (psychotic) depression, severe depression with suicidality, catatonia or negativism, agitation, complicating comorbidity, bipolar depression, or treatment resistance.